Upper Limb Amputation: Classification, Anatomy, and Prosthetic Solutions
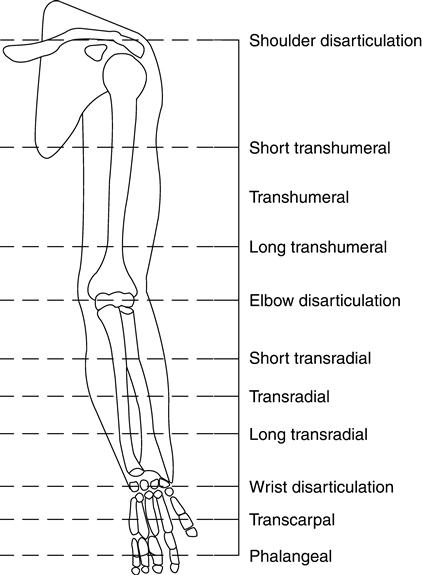
Classification of Upper Extremity Amputation Levels
Upper extremity amputations, though less common than lower extremity amputations, present unique challenges in rehabilitation, functionality, and prosthetic design. One of the most critical aspects of prosthetic management is understanding and classifying the level of amputation. The classification system for upper limb amputations is based on the anatomical level at which the limb has been lost, ranging from partial finger amputations to disarticulations at the shoulder. Each level has distinct functional implications and requires a customized prosthetic solution to optimize the user’s abilities.
1. Partial Hand Amputation
This involves the loss of one or more fingers or part of the hand, excluding the wrist. These amputations include fingertip, digital, ray, or metacarpal loss. Prosthetic solutions may be passive cosmetic devices or functional body-powered or myoelectric partial-hand prostheses. These devices aim to restore grip and support hand-based activities.
2. Wrist Disarticulation
In wrist disarticulation, the hand is removed at the wrist joint. The residual limb typically has good rotational control and a long lever arm, which is advantageous for prosthetic control. Prostheses for this level include wrist units and terminal devices (such as hands or hooks) that are either body-powered or myoelectric.
3. Transradial Amputation (Below-Elbow)
This level involves amputation between the wrist and elbow. It is one of the most common upper extremity amputation levels. A longer residual limb allows for better control and prosthetic suspension. Transradial prostheses may include cable-operated hooks or hands or more advanced myoelectric options offering improved dexterity and aesthetics.
4. Elbow Disarticulation
Elbow disarticulation entails the removal of the forearm at the elbow joint. Although the residual limb is relatively long, fitting a prosthetic elbow and forearm becomes more complex due to alignment and cosmetic concerns. However, the presence of a full humeral condyle helps with rotational control and load transmission.
5. Transhumeral Amputation (Above-Elbow)
This level involves amputation between the shoulder and elbow. The loss of the elbow joint significantly reduces the range of motion and functional potential, requiring a prosthetic elbow joint. Control systems for transhumeral prostheses may be body-powered, hybrid, or fully myoelectric. Prosthetic fitting at this level is more complex and requires training and adaptation.
6. Shoulder Disarticulation
Shoulder disarticulation refers to the removal of the entire arm at the shoulder joint. There is no residual limb for suspension, which poses challenges in prosthetic attachment and control. Prostheses for this level often involve harness systems and may incorporate shoulder joints and powered components for elbow and hand functions.
7. Forequarter Amputation (Interscapulothoracic)
This is the most extensive type of upper extremity amputation, involving removal of the arm, scapula, and part of the clavicle. Prosthetic options are limited and often used more for cosmetic purposes, though some functional systems exist. Fitting and wearing these prostheses require significant support and patient adaptation.
Conclusion: Amputation Level & Prosthetic Outcomes
The classification of upper extremity amputations is essential in guiding the selection and design of prosthetic devices. Each amputation level brings unique anatomical and functional challenges that impact prosthetic function, user control, and rehabilitation outcomes. Understanding these classifications enables clinicians and prosthetists to provide the most appropriate solutions tailored to the individual’s needs. Technological advancements, such as myoelectric control and lightweight materials, continue to enhance prosthetic options, especially for complex amputation levels. Nonetheless, patient education, training, and interdisciplinary care remain critical to achieving optimal outcomes. With proper classification and individualized treatment planning, upper limb prosthetic users can regain a significant degree of independence and quality of life.
Medical & Anatomical Considerations for Upper Limb Prosthetics
Upper extremity prosthetics represent a complex intersection of medicine, biomechanics, engineering, and human anatomy. For successful prosthetic rehabilitation, it is essential to consider several medical factors, understand the applied anatomy of the upper limb, and address underlying or associated pathological conditions. These considerations significantly influence the selection, fitting, and long-term use of prosthetic devices.

Applied Anatomy of the Upper Limb
The upper limb consists of the shoulder girdle, arm (humerus), forearm (radius and ulna), wrist, hand, and fingers. Understanding this anatomy is vital when designing prosthetic limbs that aim to restore functional movement.
Each joint in the upper extremity allows specific ranges of motion:
- The shoulder provides rotational and circumduction movements.
- The elbow allows flexion-extension and limited rotation.
- The wrist and hand provide fine motor control, critical for daily tasks.
Nerve distribution, particularly of the brachial plexus, is critical in upper limb function. Damage or amputation involving these nerves impacts both sensation and motor control, which directly affects the type of prosthetic system that can be employed—whether body-powered, myoelectric, or hybrid.
Medical Considerations for Prosthetic Fitting
When managing an upper extremity amputation, several medical factors must be evaluated before prosthetic fitting:
1. Residual Limb Health
The condition of the residual limb (stump) affects prosthetic use. Issues such as poor skin integrity, edema, scarring, neuromas, or bone spurs can interfere with socket fitting and cause discomfort or pain.
2. Pain Management
Many amputees suffer from phantom limb pain or residual limb pain, both of which must be addressed to ensure successful prosthetic rehabilitation. Treatments may include medications, desensitization therapy, or mirror therapy.
3. Muscle and Skeletal Integrity
Muscle reattachment and stabilization during surgical amputation (myodesis or myoplasty) determine the ability to control the prosthetic limb. Muscle strength and range of motion must be preserved and strengthened through physical therapy.
4. Infection and Wound Healing
In cases of traumatic or surgical amputation, preventing infection and ensuring proper wound healing is a primary medical concern. Delayed healing can postpone prosthetic fitting and functional training.
5. Patient Comorbidities
Conditions like diabetes, peripheral vascular disease, or rheumatoid arthritis can affect healing, residual limb health, and overall rehabilitation potential. These need continuous monitoring throughout prosthetic use.
Pathological Conditions Leading to Upper Limb Amputation
Several conditions may result in the need for an upper limb prosthesis:
- Trauma: The most common cause of upper limb amputation, particularly in industrial or military settings.
- Malignancies: Tumors such as osteosarcoma may necessitate amputation to prevent metastasis.
- Infections: Severe infections like necrotizing fasciitis or osteomyelitis may require surgical removal.
- Congenital Limb Deficiencies: Some individuals are born with partial or missing limbs due to developmental abnormalities.
- Vascular Disease: Less common in upper limbs than in lower limbs, but in rare cases may require amputation.
Each of these conditions presents unique challenges that influence prosthetic design, functional goals, and rehabilitation strategies.
Conclusion: Integrated Approach to Upper Limb Prosthetics
Successful prosthetic rehabilitation in upper extremity amputees requires a comprehensive understanding of medical considerations, applied anatomy, and underlying pathological conditions. The functional complexity of the upper limb necessitates a tailored approach to each patient, considering nerve integrity, residual limb condition, pain management, and comorbidities. Moreover, the cause of amputation—whether trauma, disease, or congenital—shapes the prosthetic intervention and overall rehabilitation plan. Advances in surgical techniques, prosthetic technologies (like myoelectric limbs), and multidisciplinary care continue to improve outcomes for upper limb amputees. By addressing the anatomical and medical complexities involved, clinicians can help patients achieve greater independence, mobility, and quality of life.
