Understanding Physical Medicine and Rehabilitation: Prosthetics and Orthotics
Q. Introduction to Physical Medicine & Rehabilitation:
Sure! Here’s a 500-word long, detailed answer to the question:
Q. Introduction to Physical Medicine & Rehabilitation in Detail – Prosthetics & Orthotics
Physical Medicine and Rehabilitation (PM&R), also known as Physiatry, is a specialized branch of medicine that focuses on restoring function, improving mobility, reducing pain, and enhancing the quality of life in individuals who have experienced physical impairments or disabilities. These impairments may result from conditions such as stroke, spinal cord injury, amputation, traumatic brain injury, musculoskeletal disorders, or congenital anomalies. PM&R aims to help individuals regain as much independence as possible in their daily lives through a multidisciplinary approach that includes medical management, therapy, and the use of assistive devices like prosthetics and orthotics.
The core philosophy of PM&R is functional restoration rather than only disease cure. Unlike other specialties that focus on specific organs or systems, PM&R deals with the whole person and emphasizes holistic care, including physical, emotional, psychological, and social well-being.
The rehabilitation team typically includes a physiatrist (PM&R physician), physical therapist, occupational therapist, speech-language pathologist, prosthetist, orthotist, psychologist, social worker, and rehabilitation nurse. Each team member contributes specialized knowledge to assess the patient’s needs and develop a comprehensive rehabilitation plan.
An important aspect of PM&R is the use of prosthetics and orthotics. These are external devices used to enhance the physical function of patients with limb loss, weakness, or musculoskeletal deformities.
Prosthetics
Prosthetics is the science of creating and fitting artificial limbs (called prostheses) to replace lost body parts due to amputation, trauma, cancer, or congenital absence. Prostheses can be for the upper limb (hand, forearm, elbow) or lower limb (foot, leg, knee, thigh). The primary goal of prosthetic rehabilitation is to restore as much functional ability as possible, allowing the patient to walk, perform tasks, and regain independence.
Prostheses may be cosmetic, mechanical, or myoelectric (controlled by electrical signals from residual muscles). Fitting a prosthesis involves assessment of the residual limb, fabrication of a custom socket, training in use, and continuous follow-up for adjustments.
Orthotics
Orthotics refers to the design and application of orthoses – external devices used to support, align, prevent, or correct deformities or to improve the function of a body part. These are commonly used in conditions such as stroke, cerebral palsy, polio, scoliosis, arthritis, and fractures.
Examples include ankle-foot orthoses (AFOs) for foot drop, knee-ankle-foot orthoses (KAFOs) for paralysis, wrist-hand orthoses for weak grip, and spinal braces for scoliosis. Orthoses help to improve posture, assist movement, prevent contractures, and reduce pain.
Conclusion
In conclusion, Physical Medicine and Rehabilitation plays a vital role in improving the functional outcomes and quality of life for individuals with physical disabilities. The use of prosthetic and orthotic devices is a key component of rehabilitation, helping patients regain mobility, independence, and confidence. With the support of a multidisciplinary team and advancements in technology, PM&R continues to empower individuals to overcome their physical challenges and live fuller lives.
Let me know if you’d like this in PDF format, or adapted for a presentation or handwritten notes.
Q. Muscle Charting;
Here’s a 500-word detailed answer to the question:
Q. Muscle Charting in Prosthetics & Orthotics – Detailed Explanation (500 Words)
Muscle charting is a vital assessment tool used in the field of prosthetics and orthotics as part of the comprehensive rehabilitation process. It involves the systematic evaluation of muscle strength and function in individuals with physical impairments or limb loss. Accurate muscle charting helps clinicians, especially physiatrists, physical therapists, prosthetists, and orthotists, to make informed decisions regarding the design, prescription, and fitting of prosthetic and orthotic devices.
✅ Purpose of Muscle Charting
Evaluate muscle strength and identify weakness or paralysis.
Determine functional capacity of the residual limb or affected limb.
Guide the selection of appropriate prosthetic or orthotic components.
Monitor progress during rehabilitation.
Prevent complications like contractures and joint instability.
✅ Manual Muscle Testing (MMT)
The most common method of muscle charting is Manual Muscle Testing (MMT). It grades muscle power on a scale from 0 to 5, known as the Oxford Scale:
| Grade | Muscle Strength | Description |
|---|---|---|
| 0 | Zero | No contraction visible or palpable |
| 1 | Trace | Flicker of contraction, no movement |
| 2 | Poor | Full movement with gravity eliminated |
| 3 | Fair | Full movement against gravity |
| 4 | Good | Movement against some resistance |
| 5 | Normal | Full strength against full resistance |
✅ Muscle Charting in Prosthetics
In patients with amputations, muscle charting is crucial to assess the strength of residual limb muscles, which control and support the prosthetic device.
Upper limb prosthetics: Muscle testing helps determine suitability for myoelectric prostheses, which rely on residual muscle signals for function.
Lower limb prosthetics: Muscle strength, especially in the hip extensors, flexors, and abductors, is important for prosthetic gait and balance.
Helps in choosing between passive, mechanical, or powered components based on strength.
✅ Muscle Charting in Orthotics
In orthotic management, muscle charting guides the type and level of support required. It helps determine whether a limb can be supported, mobilized, or needs to be immobilized.
Examples:
In foot drop due to weak dorsiflexors (e.g., tibialis anterior), muscle charting may indicate the need for an ankle-foot orthosis (AFO).
In paraplegia, weak hip or knee muscles may necessitate a KAFO (Knee-Ankle-Foot Orthosis) or HKAFO.
In upper limb weakness (e.g., radial nerve palsy), muscle charting helps in prescribing wrist-hand orthoses.
✅ Applications in Rehabilitation
Baseline muscle charting allows for goal setting in therapy.
Repeated charting monitors recovery or decline over time.
Helps avoid unnecessary fatigue in weak muscles by adjusting devices accordingly.
Aids in prevention of secondary issues like joint deformities, contractures, and pressure injuries.
✅ Conclusion
Muscle charting is an essential assessment process in the field of prosthetics and orthotics. It provides a clear understanding of muscular function, enabling clinicians to design appropriate devices and rehabilitation plans. Through methods like Manual Muscle Testing, practitioners can tailor prosthetic and orthotic interventions to individual needs, maximizing functionality, safety, and independence in daily life. Proper muscle charting supports optimal rehabilitation outcomes and enhances the quality of life for individuals with physical impairments.
Let me know if you’d like this in PDF, PowerPoint, or notebook-friendly format.
Q. Hydrotherapy
Hydrotherapy in Prosthetics and Orthotics: A Detailed Explanation
Hydrotherapy, also known as aquatic therapy, is the use of water in the treatment of different conditions, particularly for rehabilitation and physical therapy. In the context of prosthetics and orthotics, hydrotherapy plays a crucial role in improving mobility, strength, and overall quality of life for individuals who use prosthetic limbs or orthotic devices. It is a safe and effective therapeutic method that leverages the physical properties of water—such as buoyancy, hydrostatic pressure, viscosity, and temperature—to assist in rehabilitation and functional improvement.
Importance of Hydrotherapy in Prosthetics
%IMAGE_1%
For amputees using prosthetic limbs, hydrotherapy provides an excellent medium for early-stage rehabilitation as well as long-term physical fitness. The buoyancy of water reduces the effective weight of the body, allowing users to move more freely and with less stress on joints and residual limbs. This is particularly important for new amputees, as they often experience muscle atrophy, poor balance, and gait irregularities following limb loss.
Hydrotherapy allows patients to begin weight-bearing exercises much earlier than they could on land. This accelerates the process of learning how to walk with a prosthesis, improves gait symmetry, and enhances muscle reconditioning. Water-based therapy also assists in improving cardiovascular health, range of motion, and coordination—skills essential for successful prosthetic adaptation.
Prosthetic devices used during hydrotherapy sessions are often specially designed to be waterproof, corrosion-resistant, and lightweight. These can include swim-specific prostheses or all-terrain prosthetics that can withstand immersion. This enables users to gain confidence and independence, even in aquatic environments, such as pools, lakes, or oceans.
Role of Hydrotherapy in Orthotics
Orthotic users—individuals who rely on devices that support or correct musculoskeletal function, such as braces or foot orthoses—also benefit significantly from hydrotherapy. Those with neurological conditions like cerebral palsy, multiple sclerosis, or stroke often face spasticity, muscle weakness, and joint stiffness. Hydrotherapy helps reduce spasticity due to the warm water’s relaxing effect on muscles and promotes smoother and more controlled movement.
The hydrostatic pressure exerted by water aids in improving circulation, reducing swelling in the limbs, and enhancing proprioceptive feedback (the sense of body position), which is often diminished in individuals requiring orthotic support. As a result, patients experience better joint alignment and muscle engagement during therapy, which supports the goals of orthotic intervention.
Moreover, water resistance allows for strengthening exercises that are low-impact and safer for joints and bones. This is particularly useful for patients recovering from orthopedic surgeries or injuries. Water-based exercises also encourage improved posture, trunk control, and balance—key focus areas in orthotic rehabilitation.
Summary
Hydrotherapy is a highly effective and supportive therapy for individuals using prosthetic and orthotic devices. It provides a low-impact, high-benefit environment that facilitates rehabilitation, physical conditioning, and psychological well-being. Through specialized equipment and guided therapeutic techniques, hydrotherapy enhances the functional outcomes for patients, helping them regain independence, confidence, and mobility in both aquatic and terrestrial environments. As such, it remains an essential component of holistic care in prosthetic and orthotic rehabilitation.
Q. Application of the above topics in management of disabling conditions;
Application of Hydrotherapy in the Management of Disabling Conditions in Prosthetics and Orthotics
Hydrotherapy has increasingly become a valuable tool in the comprehensive management of disabling conditions, particularly when integrated with prosthetic and orthotic rehabilitation. Individuals living with disabilities—such as limb loss, cerebral palsy, stroke, spinal cord injury, or musculoskeletal deformities—often require prosthetic or orthotic support to restore function and mobility. The therapeutic application of water in such cases offers unique advantages that are not always possible through land-based therapy.
Application in Prosthetic Rehabilitation
For amputees, hydrotherapy is particularly useful in both pre-prosthetic and post-prosthetic rehabilitation phases. In the early stages post-amputation, patients often experience deconditioning, muscle weakness, phantom limb pain, and psychological trauma. Hydrotherapy offers a gentle yet effective method to begin movement and improve circulation without placing excessive strain on the healing limb. Buoyancy reduces body weight, which allows for safer, earlier weight-bearing activities and encourages mobility in individuals who may not yet be fitted with a permanent prosthesis.
Once the patient has been fitted with a prosthesis—especially a waterproof or swim prosthesis—hydrotherapy serves to improve gait training, balance, and coordination. The water’s resistance helps strengthen muscles, while hydrostatic pressure improves blood flow and reduces swelling in residual limbs. The reduced fear of falling in water also boosts confidence, which is critical in prosthetic adaptation and functional reintegration.
Patients with lower-limb amputations, in particular, benefit from gait training exercises in water as they can practice proper limb movement and posture with reduced risk of injury. Aquatic environments allow the therapist to guide the patient through walking, stair climbing, or directional changes with enhanced control and support.
Application in Orthotic Rehabilitation
For individuals using orthotic devices—such as ankle-foot orthoses (AFOs), knee-ankle-foot orthoses (KAFOs), or spinal braces—hydrotherapy supports motor learning, neuromuscular re-education, and functional improvement. Conditions such as cerebral palsy, multiple sclerosis, muscular dystrophy, and stroke often present with spasticity, poor balance, and restricted range of motion. Hydrotherapy can address these through warm water immersion, which promotes muscle relaxation and joint flexibility.
The resistance provided by water allows patients to perform strengthening and stretching exercises more efficiently and safely. Moreover, the supportive environment of water encourages patients to perform movements they might otherwise be unable to do on land. Children with neuromuscular disorders, for instance, may engage more fully in therapy through playful aquatic activities that support orthotic goals such as improving posture, balance, and limb alignment.
Hydrotherapy can also be beneficial for post-surgical patients recovering from tendon repairs or joint replacements who require temporary orthotic bracing. Water-based rehabilitation reduces joint load and enhances early mobility, which is key for faster recovery.
Conclusion
In the management of disabling conditions through prosthetic and orthotic intervention, hydrotherapy serves as a powerful adjunctive therapy. It offers a safe, adaptive, and therapeutic environment where physical function, psychological well-being, and overall quality of life can be significantly improved. By leveraging water’s natural properties—buoyancy, resistance, and warmth—hydrotherapy facilitates earlier mobility, enhances rehabilitation outcomes, and promotes long-term independence. As such, it plays an essential role in modern rehabilitation strategies for individuals with disabilities requiring prosthetic and orthotic care.
Q. Electrotherapy;
Electrotherapy in Detail (600 Words)
Electrotherapy is a therapeutic treatment method that uses electrical energy to stimulate nerves and muscles for medical purposes. It is a well-established modality in physical rehabilitation, pain management, and neuromuscular re-education. Electrotherapy has evolved significantly over the years, and today it encompasses a range of techniques and devices designed to aid recovery, reduce symptoms, and improve functional outcomes for patients with various disabling conditions.
Principles of Electrotherapy
The fundamental principle behind electrotherapy is the application of electrical currents to the body through electrodes placed on the skin. The type, frequency, intensity, and waveform of the current determine the therapeutic effect. These electrical impulses can modulate pain, enhance blood circulation, promote tissue healing, and stimulate muscle contractions.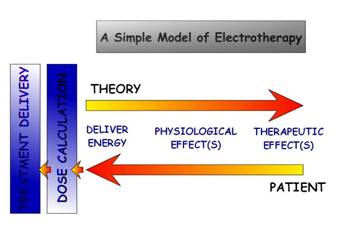
Types of Electrotherapy
1. Transcutaneous Electrical Nerve Stimulation (TENS):
TENS is primarily used for pain relief. It works by delivering low-voltage electrical impulses through the skin to stimulate sensory nerves. These impulses block pain signals from reaching the brain and stimulate the release of endorphins, the body’s natural painkillers. TENS is commonly used for conditions like arthritis, chronic back pain, neuropathy, and postoperative pain.
2. Neuromuscular Electrical Stimulation (NMES):
NMES involves the stimulation of motor nerves to cause muscle contraction. This is particularly useful in patients with muscle atrophy due to immobilization, stroke, or spinal cord injury. It helps maintain muscle tone, prevent contractures, and re-educate muscles following disuse or neurological damage.
3. Functional Electrical Stimulation (FES):
FES is a more advanced form of NMES where electrical stimulation is applied in a coordinated manner to produce functional movements. It is commonly used in patients with spinal cord injuries or after strokes to enable tasks like walking or grasping objects. FES devices can be integrated into orthotic systems to support mobility and independence.
4. Interferential Therapy (IFT):
IFT uses medium-frequency electrical currents that intersect within the body to provide deep tissue stimulation. It is effective in reducing pain, swelling, and inflammation and is often used for musculoskeletal conditions, such as osteoarthritis, ligament injuries, and post-surgical rehabilitation.
5. Iontophoresis:
Iontophoresis delivers medications transdermally (through the skin) using a mild electrical current. It is often used for localized conditions such as tendinitis, bursitis, and plantar fasciitis. Anti-inflammatory drugs like dexamethasone are commonly used in this method.
6. High-Voltage Pulsed Current (HVPC):
HVPC is used in wound healing and edema management. The high-voltage current can stimulate tissue repair, improve circulation, and reduce inflammation. It is particularly beneficial for chronic wounds, ulcers, and post-traumatic edema.
Clinical Applications
Electrotherapy is widely used in physiotherapy and rehabilitation clinics. In orthotic rehabilitation, electrotherapy can improve muscle strength and neuromuscular coordination, thus enhancing the effectiveness of orthotic devices. For example, NMES may be used to improve dorsiflexion in a patient using an ankle-foot orthosis (AFO).
In prosthetic rehabilitation, electrotherapy helps in conditioning the residual limb, controlling phantom limb pain, and preparing muscles for prosthetic control. FES, in particular, is instrumental in restoring voluntary movement in individuals with partial paralysis.
Electrotherapy is also used to treat:
Sports injuries (sprains, strains)
Post-surgical recovery
Peripheral nerve injuries
Joint contractures
Spasticity and muscle imbalances in neurological conditions
Advantages of Electrotherapy
Non-invasive and drug-free.
Conclusion
Electrotherapy is a powerful and versatile tool in modern rehabilitation medicine. By applying controlled electrical stimulation, it helps in pain relief, muscle activation, wound healing, and functional recovery. When used alongside prosthetic and orthotic interventions, electrotherapy enhances outcomes by improving muscular control, reducing pain, and facilitating faster return to functional independence. With ongoing advancements in technology and research, electrotherapy continues to expand its role in the comprehensive management of various disabling conditions, offering hope and improved quality of life to countless individuals.
Q. Neuromuscular Diseases Type and Management;
Neuromuscular diseases (NMDs) are a group of disorders that affect the nerves and muscles, leading to progressive weakness, muscle atrophy, loss of motor control, and functional disability. These conditions can be inherited or acquired and often involve the motor neurons, peripheral nerves, neuromuscular junction, or the muscle fibers themselves.
In the field of prosthetics and orthotics, managing neuromuscular diseases is essential to maintain mobility, prevent deformities, and optimize independence through the use of external support devices and rehabilitation strategies.
🔷 Types of Neuromuscular Diseases
✅ 1. Muscular Dystrophy (MD)
A group of genetic disorders characterized by progressive muscle weakness and wasting.
Examples: Duchenne Muscular Dystrophy (DMD), Becker Muscular Dystrophy
✅ 2. Spinal Muscular Atrophy (SMA)
A genetic disease affecting the anterior horn cells in the spinal cord, leading to muscle weakness and atrophy, especially in children.
✅ 3. Amyotrophic Lateral Sclerosis (ALS)
Also known as motor neuron disease (MND), it causes degeneration of upper and lower motor neurons, leading to progressive weakness.
✅ 4. Charcot-Marie-Tooth Disease (CMT)
A hereditary neuropathy affecting peripheral nerves, leading to muscle weakness, especially in the lower legs and feet.
✅ 5. Myasthenia Gravis
An autoimmune disorder affecting the neuromuscular junction, causing fatigue and weakness of voluntary muscles.
✅ 6. Post-Polio Syndrome
Occurs years after the initial poliomyelitis infection, leading to renewed muscle weakness and fatigue.
🔷 Orthotic Management
Orthoses are often the first line of support in neuromuscular diseases due to progressive muscle weakness.
▶️ Common Orthoses Used:
Ankle-Foot Orthosis (AFO)
For foot drop or weak dorsiflexion (e.g., CMT, post-polio)
Prevents tripping and improves gait pattern
Knee-Ankle-Foot Orthosis (KAFO)
For knee instability or quadriceps weakness (e.g., post-polio, SMA)
Provides full leg support
Hip-Knee-Ankle-Foot Orthosis (HKAFO)
For severe bilateral lower limb weakness (e.g., muscular dystrophy)
Spinal Orthoses (TLSO, LSO)
Used in scoliosis management (e.g., in DMD and SMA)
Upper Limb Orthoses
Wrist-hand orthosis (WHO) for weak grip
Elbow or shoulder orthoses for joint support
🔷 Prosthetic Management
In some neuromuscular diseases (e.g., advanced diabetes with neuropathy or post-polio syndrome), amputation may occur due to complications like ulcers or trauma.
▶️ Prosthetic Devices:
Transtibial or transfemoral prostheses may be needed
Lightweight and energy-efficient components are preferred
🔚 Conclusion
Neuromuscular diseases are chronic, often progressive conditions that lead to severe functional limitations. However, with timely and appropriate prosthetic and orthotic interventions, patients can maintain mobility, reduce disability, and improve quality of life. Management requires a team-based approach, individualized care, and regular reassessment to adapt devices as the disease progresses. The role of prosthetics and orthotics in such care is critical for achieving long-term independence and support.
