Spinal Orthotics: Treatments, Brace Types, and Biomechanics
Orthotic Treatment for Lumbar and Thoracic Conditions
Spinal orthoses, or back braces, play a critical role in the non-surgical management of various thoracic and lumbar spine conditions. These devices are designed to support, align, prevent or correct deformities, and improve function. Orthotic treatment is commonly prescribed for conditions such as scoliosis, kyphosis, spondylolisthesis, herniated discs, and post-surgical stabilization. The selection of the appropriate orthosis depends on the location, severity, and type of spinal pathology, as well as the patient’s age, physical activity level, and overall health status.
Lumbar Orthoses
Lumbar spine conditions often result in lower back pain, which can arise from degenerative disc disease, muscle strain, spinal stenosis, or post-operative recovery. Lumbar orthoses, such as the lumbosacral orthosis (LSO), are commonly used to manage these conditions. LSOs provide compression and restrict motion in the lumbar region, promoting healing and reducing pain. By limiting flexion, extension, and rotation, these braces help stabilize the spine and reduce stress on the intervertebral discs and facet joints.
In patients recovering from lumbar fusion surgery, orthoses are used to support the spine during the healing process. In cases of spondylolisthesis—a condition where one vertebra slips forward over the one below—an LSO can reduce excessive motion and alleviate symptoms. Additionally, LSOs are used in the treatment of compression fractures due to osteoporosis, especially in elderly populations, offering pain relief and spinal support.
Thoracic Orthoses
For thoracic spine conditions such as kyphosis or scoliosis, thoracolumbosacral orthoses (TLSOs) are the primary form of orthotic intervention. These braces typically extend from the upper back to the pelvis and are designed to control spinal curvature and maintain alignment. TLSOs are crucial in managing adolescent idiopathic scoliosis, helping to prevent curve progression in growing children and teens. The effectiveness of TLSO braces depends significantly on compliance and the degree of curvature at the start of treatment.
In kyphotic deformities, especially those associated with Scheuermann’s disease, TLSOs can correct postural deformities and relieve back pain. These braces are also indicated in post-operative spinal fusion patients to ensure proper alignment during the healing process and to limit excessive motion that could disrupt surgical repair.
Types of Braces
There are several types of spinal orthoses, including rigid, semi-rigid, and soft braces. Rigid braces, like the Boston brace or Milwaukee brace, are commonly used for scoliosis and provide three-point pressure to correct spinal curves. Soft braces are used more for support and pain relief in conditions like muscle strain, rather than for structural correction.
Orthotic Treatment for Cervical Conditions
The cervical spine, consisting of the first seven vertebrae in the neck (C1–C7), plays a crucial role in supporting the head, facilitating movement, and protecting the spinal cord. Due to its mobility and structural complexity, the cervical spine is susceptible to various conditions, including trauma, degenerative diseases, post-surgical instability, and neurological disorders. Orthotic treatment using cervical orthoses is a common and effective non-surgical approach for managing many of these conditions by providing support, immobilization, and pain relief.

Common Conditions Requiring Cervical Orthoses
- Cervical Spine Trauma: This includes fractures, dislocations, or ligamentous injuries resulting from accidents or falls. Immobilization is essential to prevent further damage to the spinal cord and to allow healing.
- Degenerative Disc Disease: As discs in the cervical spine degenerate, patients may experience pain, stiffness, and nerve compression. Orthoses can help reduce motion and relieve symptoms.
- Post-Surgical Stabilization: After spinal surgeries such as cervical fusion, orthoses are used to maintain alignment and support healing.
- Cervical Spondylosis: Age-related wear and tear on spinal discs and joints can cause chronic neck pain and stiffness.
- Neurological Disorders: Conditions like amyotrophic lateral sclerosis (ALS) or muscular dystrophy can lead to weakened neck muscles, requiring supportive orthoses.
Types of Cervical Orthoses
- Soft Cervical Collars: Made from foam and covered in fabric, soft collars provide minimal support. They are generally used for short-term pain relief in minor injuries like muscle strain or whiplash. These collars allow limited motion and help reduce muscle spasms by providing warmth and tactile feedback.
- Rigid Cervical Collars: Examples include the Philadelphia collar, Miami J collar, and Aspen collar. These offer more substantial support by restricting flexion, extension, and lateral movement. Rigid collars are typically used in moderate to severe conditions, such as stable cervical fractures or post-operative care.
- Cervicothoracic Orthoses (CTOs): These extend from the head down to the upper thoracic spine and provide more extensive immobilization than collars alone. Devices like the Sterno-Occipital Mandibular Immobilizer (SOMI) or Minerva brace are used in cases of cervical instability, complex fractures, or post-surgical recovery where maximum immobilization is necessary.
Benefits and Considerations
Orthoses reduce mechanical stress on injured structures, minimize motion, and promote healing. They also help manage pain, improve posture, and prevent deformity. In neurological cases, they provide head support when the neck muscles are too weak to maintain normal alignment. However, prolonged use without medical supervision can lead to complications such as muscle atrophy, skin irritation, and dependency. Therefore, orthotic treatment should be closely monitored by healthcare professionals and paired with physical therapy when appropriate.
Principles of Spinal Orthotic Prescription

Spinal orthoses are externally applied devices used to support, align, prevent, or correct deformities of the spine, or to improve the function of the spinal structures. The prescription of spinal orthotics requires a careful and detailed understanding of the patient’s condition, the biomechanical principles involved, and the specific goals of treatment. Whether the goal is immobilization, stabilization, correction of deformity, or pain relief, an accurate orthotic prescription plays a crucial role in the successful conservative management of spinal disorders.
Indications for Spinal Orthotics
Spinal orthoses may be prescribed for a range of conditions, including:
- Trauma (e.g., vertebral fractures)
- Post-operative immobilization
- Spinal deformities such as scoliosis and kyphosis
- Degenerative diseases, like spondylosis or disc degeneration
- Neuromuscular conditions (e.g., muscular dystrophy, ALS)
- Spinal instability due to ligament damage or disease
Each spinal region—cervical, thoracic, lumbar, or sacral—has specific orthoses tailored to address the biomechanics of that area.
Key Components of an Orthotic Prescription
A proper spinal orthotic prescription includes several essential elements:
- Diagnosis and Objectives: A clear diagnosis is necessary to define the therapeutic goals—such as limiting motion, supporting weakened structures, correcting alignment, or alleviating pain.
- Type of Orthosis: Based on the region and goal, clinicians may choose from cervical orthoses (e.g., soft collars, rigid collars like Philadelphia, SOMI), thoracolumbosacral orthoses (TLSOs) for scoliosis, kyphosis, or fractures, and lumbosacral orthoses (LSOs) for lumbar instability or disc-related pain. The choice may also be between custom vs. prefabricated devices, depending on fit and complexity.
- Design Specifications: The prescription may include details about materials (rigid or semi-rigid), control of motion (flexion, extension, lateral bending, rotation), and any special modifications.
- Duration and Use: The frequency and duration of wear are determined based on the severity of the condition and the type of orthosis. Some braces are worn full-time (e.g., scoliosis braces during growth spurts), while others may be worn during specific activities (e.g., lifting).
- Monitoring and Follow-up: Regular assessment is critical to evaluate fit, patient compliance, skin integrity, and effectiveness. Adjustments may be required over time to accommodate changes in anatomy or condition progression.
Challenges in Orthotic Prescription
Although spinal orthotics offer significant benefits, improper use or poor-fitting devices can cause discomfort, skin breakdown, or even worsen the condition. Patient compliance is also a major factor; orthoses must be as comfortable and functional as possible to ensure proper usage. Educating patients on proper application, hygiene, and the purpose of the device improves adherence and outcomes.
The Milwaukee Brace (CTLSO)

The Milwaukee brace, also known as the M.W. brace, is a type of cervico-thoraco-lumbo-sacral orthosis (CTLSO) and is one of the most well-known and historically significant spinal orthoses used in the conservative management of spinal deformities. Developed in the 1940s by Dr. Walter Blount and Dr. Albert Schmidt in Milwaukee, Wisconsin, the brace was originally designed to treat scoliosis and other spinal curvatures such as kyphosis and Scheuermann’s disease. Although newer braces have been developed since, the Milwaukee brace remains a valuable tool in specific clinical situations, particularly for high thoracic and cervicothoracic spinal curves.
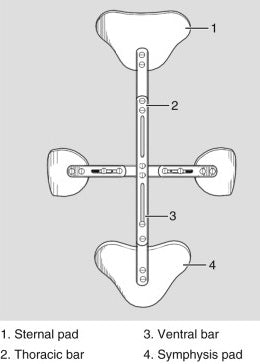
Design and Components
The Milwaukee brace is a full-torso brace that extends from the pelvis to the base of the skull. It includes the following components:
- Pelvic section: A custom-molded base that fits around the pelvis and lower torso, providing foundational support.
- Metal uprights (rods): Vertical metal bars (usually two posterior and one anterior) that connect the pelvic section to the upper part of the brace.
- Neck ring: A metal or plastic ring that encircles the neck, with chin and occipital supports to limit head and neck motion.
- Corrective pads: Positioned along the trunk, these apply pressure to the areas of spinal curvature to gradually shift the spine toward normal alignment.
- Straps and fasteners: Used to secure the brace and adjust pressure as needed.
Indications and Clinical Use
The Milwaukee brace is primarily indicated for:
- Adolescent idiopathic scoliosis with curves located in the high thoracic region (apex above T7), where lower-profile braces like the Boston brace may be ineffective.
- Kyphosis, particularly Scheuermann’s kyphosis, when the curvature is severe or located in the upper thoracic spine.
- Post-operative support after spinal surgery involving upper thoracic regions.
The brace is most effective in growing adolescents, where curve progression can be halted or reduced during critical skeletal development periods. To achieve optimal results, patients are often instructed to wear the brace for 20 to 23 hours per day, removing it only for hygiene and physical therapy.
Benefits and Limitations
The Milwaukee brace has proven effective in reducing the progression of spinal curves when used appropriately and with patient compliance. It provides three-point pressure correction and total-contact support, which can significantly improve outcomes in complex spinal deformities. However, the brace is often considered bulky and cosmetically unappealing, leading to poor compliance, particularly among teenagers. Discomfort, skin irritation, and social stigma are common barriers. As a result, newer braces like the Boston brace or Charleston bending brace are more commonly used today for lower thoracic or lumbar curves due to their more discreet design.
Essential Exercises for Milwaukee Brace Users
The Milwaukee brace (M.W. brace) is a high-profile spinal orthosis used to manage spinal deformities such as adolescent idiopathic scoliosis, kyphosis, and Scheuermann’s disease. While the brace is effective in achieving mechanical correction, its prolonged use can lead to muscle deconditioning, postural imbalances, and restricted mobility. To counteract these effects, a carefully designed exercise program is essential. Exercise during Milwaukee brace treatment is not merely complementary—it is foundational. The goals are to maintain muscle strength, joint flexibility, lung function, and psychological well-being while the spine is being corrected by the orthosis.
Stretching and Flexibility Exercises
Wearing the brace for extended hours may lead to stiffness in the spine, hips, and shoulders. Stretching helps preserve joint range of motion and prevents muscular tightness. It is recommended to perform stretching exercises twice a day, especially after removing the brace.
- Side Bends (performed out of the brace): Improves flexibility of the lateral trunk muscles.
- Hamstring and Hip Flexor Stretches: Counteract shortened muscles that can develop from long hours of sitting or bracing.
- Shoulder Rolls and Chest Openers: Prevent tightness and encourage full shoulder mobility.
- Neck Range of Motion Exercises (done gently): Help maintain cervical flexibility limited by the brace’s neck ring.
Strengthening Exercises
While the brace offers external support, the body’s core and spinal muscles must remain active and strong to maintain long-term spinal health and posture. Strength training should be supervised by a physiotherapist to ensure proper form.
- Abdominal Bracing and Pelvic Tilts: Build foundational core strength.
- Bird-Dog Pose: Enhances trunk stability while promoting coordinated movement.
- Prone Back Extensions (out of brace): Strengthens the posterior chain—important for correcting kyphosis.
- Wall Angels: Performed against a wall, these help reinforce proper shoulder and spinal alignment.
Breathing and Pulmonary Exercises
The brace’s high design can restrict chest expansion, leading to shallow breathing and decreased lung capacity. Breathing exercises promote better oxygenation and support thoracic mobility and should be performed multiple times daily, even while wearing the brace.
- Diaphragmatic Breathing: Encourages deeper abdominal breaths rather than shallow chest breathing.
- Lateral Rib Breathing: Focuses on expanding the ribcage outward with each breath.
- Balloon Blowing or Straw Breathing: Fun and effective ways, especially for children, to train deeper breathing.
Postural Training and Balance Exercises
Prolonged brace wear can affect posture awareness and balance. Exercises that restore proprioception and reinforce spinal alignment are crucial.
- Mirror Posture Drills: Standing in front of a mirror to check and correct posture.
- Single-Leg Balance: Helps develop core control and balance.
- Wall Slides and Posture Holds: Reinforce proper upright alignment.
Cardiovascular and Functional Activities
Engaging in low-impact cardio helps maintain general fitness and body coordination.
- Swimming: Excellent for symmetry, muscle balance, and spinal decompression.
- Stationary Biking and Walking: Improve circulation and endurance.
- Dance or Light Aerobics (under supervision): Promotes movement confidence and enjoyment.
The Boston Brace (TLSO)
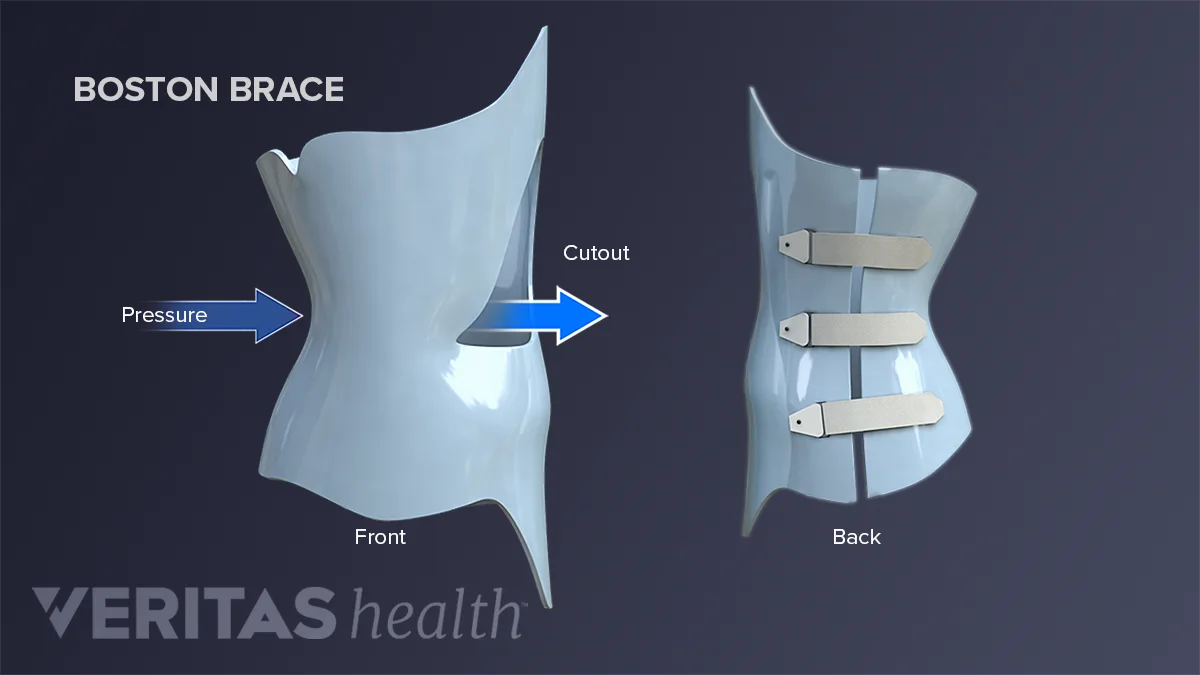
The Boston brace is one of the most widely used spinal orthoses for the conservative treatment of adolescent idiopathic scoliosis (AIS). Developed in the early 1970s at The Boston Children’s Hospital, it is a thoraco-lumbo-sacral orthosis (TLSO) that provides corrective pressure to the spine to reduce or halt the progression of spinal curves during periods of rapid growth. As a low-profile brace, it is often preferred for its ability to fit discreetly under clothing, increasing compliance among teenagers—a key factor in treatment success.
Design and Function
The Boston brace is typically made of rigid plastic molded to fit snugly around the torso. It extends from below the breast line to the pelvis, covering the thoracic and lumbar regions. Unlike earlier braces such as the Milwaukee brace, the Boston brace does not have a neck ring, making it less visible and more acceptable to young users. Inside the brace, foam pads are strategically placed based on the patient’s spinal curvature. These pads apply three-point pressure to the convex side of the spinal curve, encouraging realignment over time. The brace is custom-fitted using body scans or plaster molds and can be adjusted as the patient grows or as the curve improves.
Indications
The Boston brace is typically prescribed for:
- Adolescent idiopathic scoliosis, especially with curves ranging from 25° to 45°
- Neuromuscular scoliosis, in milder forms
- Post-operative support following spinal surgeries
- Kyphosis, though less commonly than for scoliosis
It is most effective in patients who are still growing, as skeletal immaturity is a key factor in the progression of scoliosis. Compliance is critical, and patients are generally advised to wear the brace for 16 to 23 hours per day, removing it only for bathing and certain activities like sports or physical therapy.
Benefits and Limitations
One of the key advantages of the Boston brace is its discreet, under-clothing design, which greatly improves social and emotional acceptance among adolescents. It is lightweight, durable, and customizable. When worn correctly and consistently, it can prevent curve progression in up to 80% of cases. However, limitations include:
- Discomfort, especially during initial wear
- Skin irritation or pressure sores if not fitted properly
- Psychological stress or body image concerns
- Limited effectiveness in curves greater than 45°, which may require surgery
Key Components of Spinal Braces

Spinal braces, also known as spinal orthoses, are externally applied devices used to support, stabilize, correct, or prevent the progression of spinal deformities and injuries. These orthotic devices are essential tools in non-surgical spinal care. Regardless of the condition being treated, all spinal braces share certain key components, each playing a crucial role in function, effectiveness, and patient comfort.
Shell or Body of the Brace
The primary component of any spinal brace is the rigid or semi-rigid shell that forms its structure. Typically made from thermoplastics like polypropylene, the shell is custom-molded to the patient’s body or adjusted from prefabricated models. This structure encases part or all of the torso. For example:
- TLSOs (Thoraco-Lumbo-Sacral Orthoses) like the Boston brace cover the thoracic and lumbar regions.
- LSOs (Lumbo-Sacral Orthoses) cover only the lower back.
- CTLSOs (Cervico-Thoraco-Lumbo-Sacral Orthoses), like the Milwaukee brace, extend from the pelvis to the base of the skull.
The shell distributes corrective and stabilizing forces over a broad area, which helps realign the spine, restrict motion, and reduce pressure on spinal structures.
Pads and Liners
Inside the brace, pressure pads are strategically placed to apply targeted forces to specific areas of the spine. These pads are often made from foam or silicone and are crucial in scoliosis treatment, where three-point pressure systems are used to push the spine toward a more neutral alignment. Liners, usually made of soft, breathable material, are placed between the skin and the brace to reduce friction, absorb sweat, and improve comfort.
Straps and Fastening Mechanisms
Straps are vital for securing the brace and ensuring it stays in the correct position. Most spinal braces use hook-and-loop (Velcro) straps, buckles, or laces. These allow for easy application and removal of the brace and enable adjustment of tightness for both comfort and effectiveness. The straps also help customize the compression applied by the brace.
Supportive Framework or Rods
Some spinal braces, particularly high-profile types like the Milwaukee brace, include metal uprights or rods that run vertically along the spine. These provide structural support and connect the pelvic section to a neck ring, offering higher-level immobilization essential in cases requiring full spinal stabilization.
Chin and Occipital Pads
In CTLSOs like the Milwaukee brace, chin and occipital pads attached to a neck ring are used to limit cervical motion. These pads provide a point of contact to guide spinal alignment and prevent the user from adopting poor posture.
Understanding the Biomechanics of the Spine

The human spine is a complex and dynamic structure composed of vertebrae, intervertebral discs, ligaments, muscles, and neural elements. Its primary functions include providing structural support, enabling flexible movement, and protecting the spinal cord. Understanding the biomechanics of the spine is essential in spinal orthotics, as it guides the design, selection, and application of braces used to correct deformities, limit movement, and promote healing.
Basic Spinal Biomechanics
The spine is divided into five regions, each with specific characteristics:
- Cervical spine (C1–C7): Supports the head and allows extensive motion.
- Thoracic spine (T1–T12): Less mobile due to rib attachments; designed more for stability.
- Lumbar spine (L1–L5): Bears the most weight; allows flexion and extension but limited rotation.
The intervertebral discs act as shock absorbers, while facet joints guide and limit movement. The spine’s natural S-shaped curve distributes mechanical loads efficiently.
Forces Acting on the Spine
The spine is constantly subjected to axial loading, shear forces, torsion, and bending moments. These forces increase during activities such as lifting or twisting. Abnormal loading can result in pain, disc degeneration, or spinal deformities like scoliosis. When a deformity is present, normal biomechanics are altered, creating asymmetric loading that can lead to further progression of the curve if not managed properly.
Role of Spinal Orthotics in Biomechanics
Spinal orthotics (braces) work by altering the biomechanical environment of the spine. They achieve their therapeutic goals by:
- Redistributing forces: Braces distribute compressive loads over a broader area, reducing stress on specific spinal segments.
- Limiting motion: By restricting certain movements, braces prevent further injury, which is critical post-surgery or during fracture healing.
- Applying corrective forces: In cases of scoliosis or kyphosis, orthoses apply targeted pressure to realign the spine through three-point force systems.
- Enhancing proprioception: Braces improve postural awareness and help patients avoid harmful movements.
By understanding the underlying biomechanics, orthotists can tailor brace design to the specific needs of the patient, ensuring maximum effectiveness.
Current Research and Advances in Spinal Orthotics

Recent publications continue to expand the scientific landscape of spinal orthotics, focusing on biomechanics, technology, and patient-centered care.
Biomechanical Foundations and Force Quantification
A systematic review in Bioengineering (December 2024) investigated interface pressures and strap tensions in braces for adolescent idiopathic scoliosis (AIS). Median pressures were reported at ~8.75 kPa on thoracic pads and ~7.11 kPa on thoracolumbar/lumbar pads, with strap tensions averaging around 42.5 N. These reference values are crucial for improving design and standardizing fitting protocols.
Advances in Brace Design: CAD/CAM Customization
The rise of CAD/CAM technology has transformed brace manufacturing. Modern braces such as the Regnier-Chêneau and Gensingen braces are designed with curve-specific customization. CAD/CAM production eliminates plaster casting, enhances precision, and improves in-brace correction, which is associated with favorable treatment outcomes.
Evidence of Brace Effectiveness in AIS
Though the landmark BrAIST trial (2013) established that wearing a brace ≥18 hours a day notably reduced progression to surgical thresholds, current research continues to support this standard. A scoping review protocol published in BMJ Open (2023) aims to synthesize systematic reviews on brace effectiveness up to 2023.
Evolving Focus: Patient-Centered Care
An editorial summarizing two decades of innovation highlights a shift toward evidence-based medicine and patient-centered care. There is growing attention to mental health, quality of life, and automated assessment tools, with emerging research in underrepresented spinal deformities like Scheuermann’s hyperkyphosis.
Adult Scoliosis: Outcomes and Harms
There is a noted scarcity of literature on the orthotic management of adult scoliosis. A systematic review of studies from 1967 to 2018 identified limited evidence about clinical outcomes and potential harms in this demographic, highlighting the need for more robust research.
Conclusion
Orthotic treatment using spinal braces is a vital component of conservative spine care. Whether used for pain management, post-operative recovery, or the correction of spinal deformities, orthoses can significantly improve quality of life and functional outcomes. The success of treatment depends on a careful prescription based on a clear diagnosis, biomechanical principles, and patient-specific factors. Advances in technology like CAD/CAM are improving brace design and effectiveness, while ongoing research continues to refine clinical standards. With proper application, monitoring, and patient adherence, spinal orthoses offer an effective non-invasive method to manage and treat a wide range of spinal disorders.
